Over the summer of 2019, Divine Mercy University (DMU) made its highly anticipated move from Crystal City, just outside of Washington D.C., to its new campus in Sterling, Virginia. In addition to the big move, DMU also brought in some new faces, including Psy.D. graduate Dr. Kristi Stefani. Originally from Montana, Dr. Stefani joined the Continue reading
clinical psychology
6 Tips for Handling Holiday Stress
We always look to the holidays as a time of celebration; a magical time of good cheer, warm traditions, and being with family and friends. We think of it as a time of rest and relaxation, filled with joy and gratitude for all that we have. Despite the surface magic and positivity, the holidays are Continue reading
Miscarriage Trauma Involves Mental Health Need
Step into an examination room at an OB-GYN, and you may find a young couple staring up at a monitor. Little by little, their pure love, joy and anticipation illuminates the room, burying any sense of worry or cautiousness they may have. But as they both stare up at the monitor–anxious to see and hear Continue reading
Unfolding the Person with Positive Psychology
This past September, the Abat Oliba CEU University in Barcelona, Spain, held the first European Congress of Christian Anthropology and Mental Health Sciences. The purpose of the congress assembly is to address the separation between mental health sciences and Christian anthropology, and to deepen the holistic vision of psychology and health sciences. Divine Mercy University’s Continue reading
DMU’s New Campus Officially Opens
Twenty years ago, a handful of students, instructors, and psychology professionals met in a small space in Arlington, VA, and began the very first semester of the Institute for the Psychological Sciences (IPS). This resulted in the launch of a new vision and mission to integrate traditional psychology into harmonized mental health science and therapy Continue reading
Remembering the Virginia Tech Shooting
The small town of Blacksburg in Southern Virginia was, at one point, only that: a small town, nestled along the New River Valley. The trip from the cities of the north will lead you witnessing the significant change of scenery as you cruise down I-81, from cityscapes to treelines, from city streets to nature trails, Continue reading
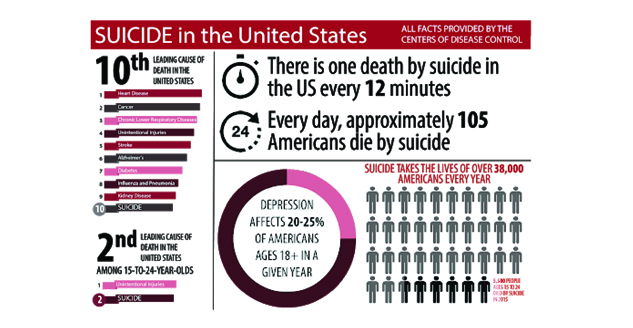
Staggering Suicide Statistics
Suicide is not a topic we all like to talk about. But recent incidents have brought more attention to this unfortunate event that’s often linked to severe depression. At Divine Mercy University, we strive to educate our students and the general public of ways to prevent suicide and provide adequate mental health services. Recently, we Continue reading
Fostering Inclusivity in Eating Disorder Awareness
Did you know that an eating disorder is a physical AND mental illness that affects people of ALL backgrounds? Instead of pigeonholing this condition to one particular category of people, National Eating Disorders Association’s Awareness Week (February 25-March 3) is fostering inclusivity this year to show how this disease impacts “individuals at all stages of body Continue reading
Stigmas Still Scare People From Counseling
What happens when we’re confronted with a problem? What do we do when we have an issue we’re trying to fix at work or trying to solve a problem in our schoolwork? What do we do when we can’t fix something at home–a jammed window, a dislodged door, a flat tire on the car? What Continue reading
Sharp Divide Overrules Mental Health
Written by Eric Kambach, Marketing Associate at Divine Mercy Universtiy. Sitting in a hospital room during an emergency, waiting to speak with a doctor builds a great anxiety that makes the heart race while simultaneously petrifying the body. Words of comfort fall over and around you like acorns in autumn, and thoughts bounce around inside Continue reading